Delving into the intricacies of HESI case study chronic renal failure, this comprehensive analysis unveils the complexities of this condition and the multifaceted role of hemodialysis in its management. Through an exploration of pathophysiology, nursing interventions, patient education, and case study analysis, this work provides a holistic understanding of this prevalent health concern.
Chronic Renal Failure (CRF) Overview: Hesi Case Study Chronic Renal Failure
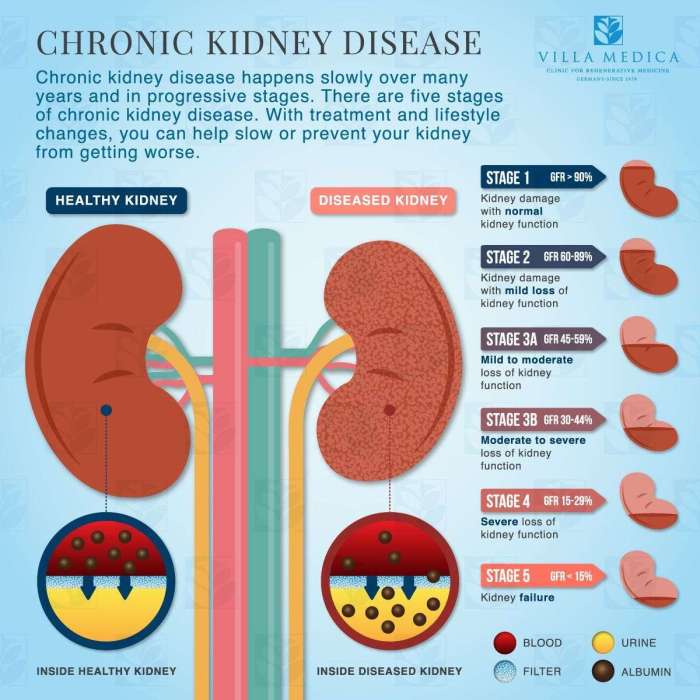
Chronic Renal Failure (CRF) is a progressive, irreversible decline in renal function characterized by a gradual loss of nephrons and impaired ability to excrete waste products and regulate fluid and electrolyte balance. It can result from various underlying diseases and conditions that cause ongoing damage to the kidneys.
CRF is a significant global health concern, affecting approximately 10% of the population worldwide. The prevalence increases with age, with older adults being at a higher risk. Diabetes and hypertension are the leading causes of CRF, accounting for more than half of all cases.
Causes
- Diabetes
- Hypertension
- Glomerulonephritis
- Obstructive uropathy
- Autoimmune diseases
- Medications and toxins
li>Polycystic kidney disease
Pathophysiology
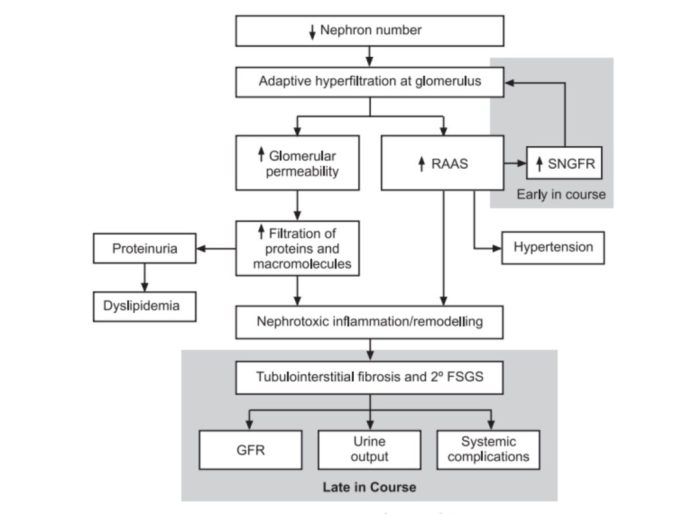
CRF occurs when the kidneys are unable to adequately filter waste products from the blood due to damage to the nephrons. This damage can lead to a build-up of toxins, fluid, and electrolytes in the body, resulting in a variety of complications.
Complications
- Anemia
- Hyperkalemia
- Metabolic acidosis
- Cardiovascular disease
- Osteoporosis
- Neurological disorders
Hemodialysis for CRF
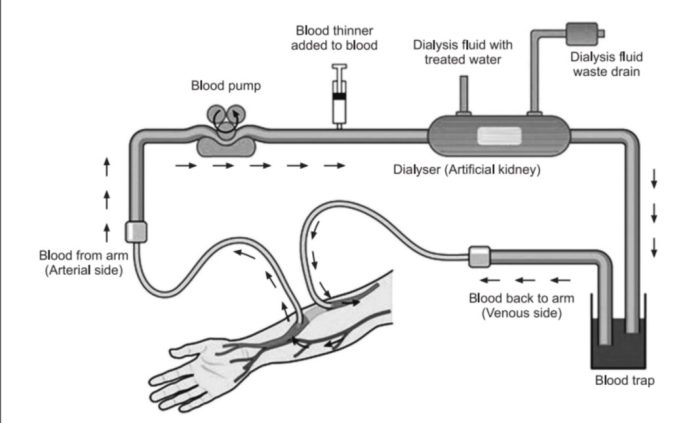
Hemodialysis is a renal replacement therapy used to treat patients with chronic renal failure (CRF) when their kidneys can no longer adequately filter waste products and excess fluid from the blood.
The principle of hemodialysis involves using a semipermeable membrane to separate waste products and excess fluid from the blood. The blood is pumped through a dialyzer, which contains the semipermeable membrane, and dialyzing fluid flows on the other side of the membrane.
The waste products and excess fluid diffuse across the membrane into the dialyzing fluid, which is then discarded.
Indications
Hemodialysis is indicated for patients with CRF who have:
- End-stage renal disease (ESRD)
- Severe fluid overload
- Hyperkalemia
- Metabolic acidosis
Benefits
Hemodialysis can provide several benefits for patients with CRF, including:
- Removal of waste products and excess fluid from the blood
- Control of blood pressure
- Correction of electrolyte imbalances
- Improvement of overall well-being
Limitations, Hesi case study chronic renal failure
Hemodialysis also has some limitations, including:
- It is a time-consuming procedure, typically requiring several hours of treatment three times per week.
- It can cause side effects such as nausea, vomiting, muscle cramps, and fatigue.
- It requires a vascular access, which can be a source of complications such as infection and thrombosis.
- It does not cure CRF and is only a temporary solution until a kidney transplant can be performed.
Nursing Management of CRF Patients on Hemodialysis
Nursing management of chronic renal failure (CRF) patients on hemodialysis is crucial to ensure optimal patient outcomes. Nurses play a vital role in managing symptoms, monitoring complications, and providing patient education to support self-management.
Assessment
Comprehensive assessment is essential to tailor nursing interventions. This includes:
- Medical history, including dialysis modality and duration
- Physical examination, focusing on fluid status, cardiovascular health, and nutritional status
- Laboratory values, including electrolytes, blood urea nitrogen (BUN), and creatinine
- Psychosocial assessment, evaluating coping mechanisms and support systems
Symptom Management
Hemodialysis can cause various symptoms, including:
- Fatigue and weakness
- Nausea and vomiting
- Muscle cramps
- Hypotension
Nursing interventions to manage these symptoms include:
- Adequate rest and hydration
- Anti-emetics for nausea
- Calcium supplements for muscle cramps
- Monitoring blood pressure and adjusting dialysis settings to prevent hypotension
Monitoring Complications
Hemodialysis patients are at risk for complications, such as:
- Infection
- Vascular access thrombosis
- Cardiovascular events
- Dialysis disequilibrium syndrome
Nurses monitor for signs and symptoms of these complications and implement appropriate interventions, including:
- Aseptic technique to prevent infection
- Regular vascular access assessment and care
- Cardiac monitoring and medications for cardiovascular events
- Slowing dialysis rate or adjusting settings to prevent dialysis disequilibrium syndrome
Patient Education
Patient education is crucial for self-management and improving outcomes. Nurses provide education on:
- Hemodialysis process and schedule
- Fluid and dietary restrictions
- Medication management
- Infection prevention
- Coping mechanisms and support systems
Patient Education and Support
Providing patients with chronic renal failure (CRF) and their families with comprehensive education and support is crucial for improving outcomes and empowering them to manage their condition effectively. A well-structured patient education program should cover various aspects of CRF, including its causes, symptoms, treatment options, and lifestyle modifications.
Empowering patients with knowledge about their condition enables them to make informed decisions regarding their treatment and lifestyle choices. Education also helps reduce anxiety, promote self-care management, and improve adherence to prescribed therapies.
Patient Education Program
A comprehensive patient education program should address the following key areas:
- Overview of CRF, its causes, symptoms, and progression
- Treatment options, including hemodialysis, peritoneal dialysis, and kidney transplantation
- Dietary modifications and fluid restrictions
- Medication management and potential side effects
- Lifestyle adjustments, such as exercise, smoking cessation, and stress management
- Importance of regular follow-up appointments and monitoring
Patient Adherence, Self-Care Management, and Support Groups
Patient adherence to prescribed treatments and lifestyle modifications is essential for successful management of CRF. Adherence can be improved through education, regular monitoring, and support from healthcare professionals and family members.
Self-care management empowers patients to take an active role in their health. It involves monitoring symptoms, adhering to medication regimens, managing fluid intake, and making appropriate dietary choices.
Support groups provide a valuable platform for patients to connect with others who are experiencing similar challenges. They offer emotional support, practical advice, and a sense of community.
Case Study Analysis
A 62-year-old male patient with a history of hypertension and diabetes mellitus was admitted to the hospital with a chief complaint of fatigue and shortness of breath. His past medical history also included a myocardial infarction 5 years ago and a stroke 2 years ago.
He had been on hemodialysis for the past 3 years due to end-stage renal disease.
On physical examination, the patient was alert and oriented. His blood pressure was 150/90 mmHg, his heart rate was 90 beats per minute, and his respiratory rate was 20 breaths per minute. He had pitting edema in his lower extremities and a jugular venous distension.
His lungs were clear to auscultation, and his heart had a regular rhythm with no murmurs or gallops.
Laboratory studies revealed a creatinine level of 10 mg/dL, a blood urea nitrogen (BUN) level of 80 mg/dL, and a potassium level of 5.5 mEq/L. His hemoglobin level was 10 g/dL, and his white blood cell count was 10,000/mm3. A chest X-ray showed cardiomegaly and pulmonary congestion.
The patient was started on hemodialysis three times per week. His symptoms gradually improved, and his laboratory values stabilized. He was discharged from the hospital after 1 week and was followed up closely in the outpatient clinic.
Challenges and Decision-Making
The patient’s case highlights several challenges and decision-making points in the management of CRF patients on hemodialysis.
- Dialysis Modality:The decision of whether to initiate hemodialysis or peritoneal dialysis is a complex one. Hemodialysis is typically preferred for patients with severe CRF who require more frequent and intensive dialysis. Peritoneal dialysis may be preferred for patients who are not candidates for hemodialysis, such as those with severe cardiovascular disease or who are unable to tolerate the anticoagulation required for hemodialysis.
- Dialysis Frequency:The frequency of hemodialysis is another important decision. The standard frequency is three times per week, but some patients may benefit from more frequent dialysis, such as daily or nocturnal hemodialysis. The frequency of dialysis is based on the patient’s individual needs and the severity of their CRF.
- Access:The creation of a vascular access is necessary for hemodialysis. There are two main types of vascular access: arteriovenous fistula (AVF) and arteriovenous graft (AVG). An AVF is a connection between an artery and a vein, while an AVG is a synthetic graft that is placed between an artery and a vein.
AVFs are typically preferred over AVGs because they have a longer lifespan and are less likely to clot.
- Medications:CRF patients on hemodialysis require a number of medications, including erythropoietin, iron supplements, calcium supplements, and phosphate binders. Erythropoietin is a hormone that stimulates the production of red blood cells. Iron supplements are necessary to prevent anemia. Calcium supplements are necessary to prevent hypocalcemia.
Phosphate binders are necessary to prevent hyperphosphatemia.
- Patient Education:Patient education is essential for CRF patients on hemodialysis. Patients need to understand the importance of adhering to their dialysis schedule, taking their medications, and following a healthy diet. They also need to be aware of the signs and symptoms of complications, such as infection, bleeding, and hypotension.
Frequently Asked Questions
What are the common causes of chronic renal failure?
Chronic renal failure can result from various causes, including diabetes, hypertension, glomerulonephritis, and polycystic kidney disease.
How does hemodialysis work in treating chronic renal failure?
Hemodialysis involves filtering waste products and excess fluid from the blood using an artificial kidney machine, providing temporary support for kidney function.
What are the potential complications associated with hemodialysis?
Hemodialysis can be associated with complications such as hypotension, muscle cramps, nausea, and infection, requiring careful monitoring and management.